Restaurant Paneer is Dangerous for Heart & Health: Say No to Artificial Paneer
Reading Time: 4 minutes Spread the love Restaurant Paneer is Dangerous for Heart & Health: Say No to Artificial Paneer. The Rising Demand for Paneer-Based Food…
Dr AvinashTank, is a super-specialist (MCh) Laparoscopic Gastro-intestinal Surgeon,
Haemorrhoids are vascular structures in the anal canal which help with stool control. They become pathological or piles when swollen or inflamed. In their normal state, they act as a cushion composed of arterio-venous channels (blood vessels) and connective tissue.
While the exact cause of hemorrhoids remains unknown, a number of factors which increase intra-abdominal pressure, i.e. prolonged straining for constipation, chronic cough, pregnancy, are believed to play a role in their development.
During pregnancy, pressure from the fetus (baby) on the abdomen and hormonal changes cause the hemorrhoidal vessels to enlarge. Delivery also leads to increased intra-abdominal pressures. Pregnant women rarely need surgical treatment, as symptoms usually resolve after delivery.

The symptoms of pathological haemorrhoids depend on the type of haemorrhoid present.
Hemorrhoids are typically diagnosed by physical examination. A visual examination of the anus and surrounding area may diagnose external or prolapsed haemorrhoids. Visual confirmation of internal hemorrhoids require Anoscopy, a hollow tube device with a light attached at one end. There are two types of haemorrhoids: external and internal. These are differentiated by their position with respect to the dentate line. A rectal exam may be performed to detect possible rectal tumors & polyps.
Internal Haemorroids
Internal haemorrhoids are those that originate above the dentate line. They are covered by columnar epithelium which lacks pain receptors, that the reason that they are painless. They were classified into four grades based on the degree of prolapse.
External Haemorroids
External hemorrhoids are those that occur below the dentate or pectinate line. They are covered proximately by anoderm and distally by skin, both of which are sensitive to pain and temperature.
The primary concern of patients with rectal bleeding is the possibility of colorectal cancer. Other diagnoses that may need to be excluded include colitis like inflammatory bowel disease, diverticular disease, and angiodysplasia. More extensive endoscopic evaluation with complete colonoscopy or flexible sigmoidoscopy is indicated in following conditions
Medical treatment includes diet rich with fibres, intake of oral fluids to maintain hydration and sitz baths.
A number of office based procedures may be performed. While generally safe, rare serious side effects such as perianal sepsis may occur.
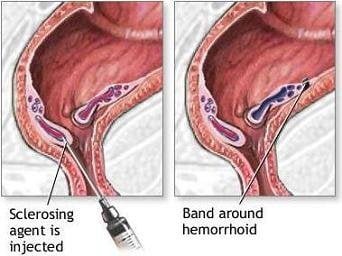
Rubber band ligation is typically recommended as the first line treatment in those with grade 1 to 3 disease. It is a procedure in which elastic bands are applied onto an internal hemorrhoid at least 1 cm above the dentate line to cut off its blood supply. Within 5″7 days, the withered hemorrhoid falls off. Cure rate has been found to be about 87% with a complication rate of up to 3%.
Sclerotherapy involves the injection of a sclerosing agent, such as phenol, into the hemorrhoid. This causes the vein walls to collapse and the hemorrhoids to shrivel up. The success rate four years after treatment is ~70% which is higher than that with rubber band ligation.
Cauterization methods: A number of cauterization methods have been shown to be effective for haemorrhoids, but are usually only used when other methods fail. This procedure can be done using electrocautery, infrared radiation, laser surgery or cryosurgery. These methods may be an option for grade 1 or 2 disease. In those with grade 3 or 4 disease re-occurrence rates are high.
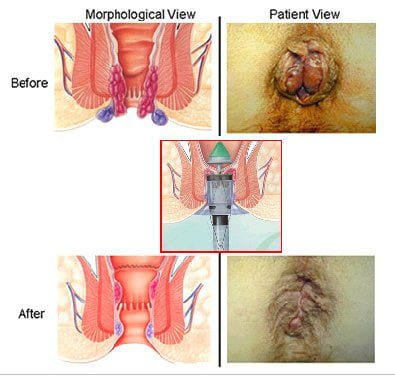
Surgical Hemorrhoidectomy should be reserved for patients refractory to office procedures or unable to tolerate office procedures, patients with large external hemorrhoids,or patients with combined internal and external hemorrhoids with significant prolapse.
Excisional hemorrhoidectomy is a surgical excision of the hemorrhoid used primarily only in severe cases. It is associated with significant post-operative pain and usually requires 2″4 weeks for recovery. However, there is greater long term benefit in those with grade 3 hemorrhoids as compared to rubber band ligation. It is the recommended treatment in those with a thrombosed external hemorrhoid if carried out within 24″72 hours.
Doppler-guided, transanal hemorrhoidal dearterialization is a minimally invasive treatment using an ultrasound doppler to accurately locate the arterial blood inflow. These arteries are then “tied off” and the prolapsed tissue is sutured back to its normal position. It has a slightly higher recurrence rate, but fewer complications compared to a hemorrhoidectomy.
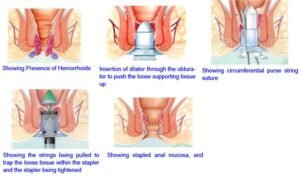
Stapled hemorrhoidectomy (stapled hemorrhoidopexy), is a procedure that involves the removal of much of the abnormally enlarged hemorrhoidal tissue, followed by a repositioning of the remaining hemorrhoidal tissue back to its normal anatomic position. It is generally less painful and is associated with faster healing compared to complete removal of hemorrhoids. However, the chance of symptomatic hemorrhoids returning is greater than for conventional hemorroidectomy and thus it is typically only recommended for grade 2 or 3 diseases. Exceptionally rare but potentially devastating complications include anovaginal fistula, substantial hemorrhage and rectal perforation and / or retroperitoneal sepsis.
Stapled haemorrhoidopexy is a new alternative available for individuals with significant haemorrhoidal prolapse. It involves a mucosal and submucosal, circular resection of the haemorrhoidal columns at their apex. In addition, the blood supply is interrupted and haemorrhoids are fixed to the distal rectal muscular wall. This is all accomplished by a single firing of a modified, circular anastomotic stapler.

Our expert team members shall help you to prepare you for surgery.
in most cases, you will need some tests before your surgery. The tests routinely used include:
Our expert team of Anaesthetist will ask you questions pertaining to your health and to assess your fitness for surgery. You are requested to tell them in detail about your current and past medical ailments, allergic reactions you’ve had in the past and current medicines that you are taking like blood thinning medicine. This medicine should be stopped prior to surgery to minimize the risk of bleeding during /after surgery.
Anaesthesia is the use of drugs to make the body unable to feel pain for a period of time. General anaesthesia puts you into a deep sleep for the surgery. It is often started by having you breathe into a face mask or by putting a drug into a vein in your arm. Once you are asleep, an endotracheal or ET tube is put in your throat to make it easy for you to breathe. Your heart rate, breathing rate, and blood pressure (vital signs) will be closely watched during the surgery. A doctor watches you throughout the procedure and until you wake up. They also take out the ET tube when the operation is over. You will be taken to the recovery room to be watched closely while the effects of the drugs wear off. This may take hours. People waking up from general anaesthesia often feel “out of it” for some time. Things may seem hazy or dream-like for a while. Your throat may be sore for a while from the endotracheal (ET) tube.
Informed consent is one of the most important parts of getting ready for surgery. It is a process during which you are told about all aspects of the treatment before you give written permission to perform the surgery.
Depending on the type of operation you have, there may be things you need to do to be ready for surgery:
You may feel pain at the site of surgery. We aim to keep you pain free after surgery with the help of latest and most effective technique or analgesic (pain relieving medicine).
You will be allowed orally liquids once you recover from effect of anaesthesia medicine and you don’t have nausea or vomiting. Gradually you can add soft to normal diet.
Our health care team will try to have you move around as soon as possible after surgery. You are encouraged to get out of bed and walk the same day. While this may be hard at first, it helps speed your recovery. It also helps your circulation and helps prevent blood clots from forming in your legs.
Once you are eating and walking, and then you are ready to go home, in most case in next day following surgery. Before leaving for home our health care team shall give you detailed guidance regarding diet, activities, medications & further plan of treatment
There are risks that go with any type of medical procedure and surgery is no longer an exception. Success of surgery depends upon 3 factors: type of disease/surgery, experience of surgeon and overall health of patients. What's important is whether the expected benefits outweigh the possible risks.
Our health care team shall advise you in detail regarding dietary habits, Briefly, your diet begins with liquids followed by gradual advance to solid foods.
Patients are encouraged to engage in light activity while at home. You will be able to get back to your normal activities within a short amount of time (week).
You may be advised to see our health care team after 1 week to assess your progress and to address your problems.

Experience
Award & Presentations
Satisfied Families
Successful Surgeries

Endoscopy
Reading Time: 4 minutes Spread the love Restaurant Paneer is Dangerous for Heart & Health: Say No to Artificial Paneer. The Rising Demand for Paneer-Based Food…
Reading Time: 4 minutes Spread the love Real vs. Fake Paneer (Analogous Paneer): How to Identify and Health Risks. Paneer is a staple in Indian households, known…
Reading Time: < 1 minute Spread the love Anti-Cancer Indian Diet. Here’s the content from the uploaded notes organized into a proper list in both Hindi…