Reading Time: 3 minutes
Why ApoB and Non-HDL Cholesterol Are Better Predictors of Cardiovascular Risk Than LDL Cholesterol.
Dr Vineet Sankhla (DM Cardiology)
Consultant interventional cardiologist
Palmerston North Hospital,
Palmerston North city,
Health New Zealand
Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality worldwide, and accurate risk prediction is essential for effective prevention and management.
While low-density lipoprotein cholesterol (LDL-C) has long been the cornerstone marker for assessing cardiovascular risk, emerging evidence highlights the superiority of apolipoprotein B (ApoB) and non-HDL cholesterol (non-HDL-C) as more comprehensive and reliable predictors of risk.
1. Understanding LDL-C, ApoB, and Non-HDL-C

•LDL-C: Refers to the cholesterol content within low-density lipoprotein particles, often termed “bad cholesterol.” It is the most commonly measured lipid parameter in clinical practice.
•ApoB: The primary structural protein of atherogenic lipoproteins, including LDL, very-low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and lipoprotein(a). Each atherogenic particle contains one ApoB molecule, making ApoB a direct measure of the number of atherogenic lipoprotein particles.
•Non-HDL-C: Calculated as total cholesterol minus HDL cholesterol. It represents the cholesterol content in all atherogenic lipoproteins, including LDL, VLDL, IDL, and chylomicron remnants.
2. Limitations of LDL Cholesterol
•Focuses Only on LDL Particles: LDL-C measures the cholesterol carried by LDL particles but does not account for other atherogenic particles like VLDL and IDL, which contribute to CVD risk.
•Does Not Reflect Particle Number: Individuals with the same LDL-C level can have varying numbers of LDL particles (LDL-P) due to differences in particle size. Smaller, denser LDL particles are more atherogenic, and LDL-C does not capture this variability.
•Affected by Metabolic Conditions: Conditions like insulin resistance, obesity, and type 2 diabetes can lead to discordance between LDL-C and actual atherogenic lipoprotein burden.
3. Advantages of ApoB as a Risk Predictor
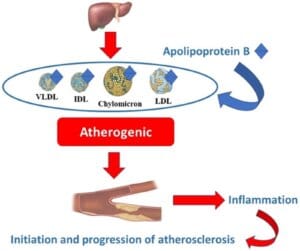
•Direct Measure of Atherogenic Particle Number: ApoB reflects the total number of atherogenic lipoproteins, including LDL, VLDL, and IDL, providing a more accurate assessment of atherogenic burden.
•Predicts Residual Risk: In studies, ApoB has been shown to predict residual cardiovascular risk even when LDL-C levels are well-controlled, making it particularly valuable in treated populations.
•Unaffected by Lipoprotein Composition: Unlike LDL-C, ApoB is not influenced by particle size or cholesterol content, making it a more stable and reliable marker across different metabolic states.
4. Advantages of Non-HDL Cholesterol
•Includes All Atherogenic Lipoproteins: Non-HDL-C encompasses the cholesterol content of LDL, VLDL, IDL, and other atherogenic particles, providing a broader measure of risk compared to LDL-C.
•Readily Available and Cost-Effective: Non-HDL-C can be calculated from a standard lipid panel without additional costs or specialized tests.
•Stronger Risk Association: Research has consistently shown that non-HDL-C correlates better with cardiovascular risk than LDL-C, particularly in individuals with elevated triglycerides or metabolic syndrome.
5. Evidence Supporting ApoB and Non-HDL-C
•Meta-analyses and Clinical Trials: Numerous studies, including large meta-analyses, have demonstrated that ApoB and non-HDL-C outperform LDL-C in predicting cardiovascular events.
•Discordance Studies: In cases where LDL-C is discordant with ApoB or non-HDL-C, ApoB and non-HDL-C better correlate with cardiovascular risk, especially in individuals with high triglycerides or diabetes.
•Guideline Endorsements: Recent guidelines from organizations like the European Society of Cardiology (ESC) and American Association of Clinical Endocrinologists (AACE) recommend the use of ApoB and non-HDL-C as supplementary or primary markers for cardiovascular risk assessment.
6. Clinical Scenarios Where ApoB and Non-HDL-C Excel
•Hypertriglyceridemia: Non-HDL-C and ApoB capture the risk posed by triglyceride-rich lipoproteins, which are not accounted for by LDL-C.
•Diabetes and Metabolic Syndrome: In these conditions, LDL-C often underestimates risk due to the presence of small, dense LDL particles and increased VLDL.
•Residual Risk in Treated Patients: Even in patients achieving LDL-C targets with statins or other lipid-lowering therapies, ApoB and non-HDL-C identify residual atherogenic risk.
7. Practical Implications
•ApoB Testing: Although not part of routine lipid panels, ApoB testing is increasingly available and recommended for high-risk individuals or when discordance is suspected.
•Non-HDL-C as a Practical Alternative: Non-HDL-C offers a cost-effective and easily accessible marker that can be calculated without additional testing.
•Integrative Approach: Combining LDL-C, ApoB, and non-HDL-C provides a more comprehensive risk assessment, especially in complex cases.
Conclusion
While LDL cholesterol has been the traditional marker for assessing cardiovascular risk, ApoB and non-HDL cholesterol offer superior predictive value by capturing the full burden of atherogenic lipoproteins.
Their ability to reflect particle number and account for diverse lipoprotein classes makes them more reliable tools for identifying and managing cardiovascular risk, especially in individuals with metabolic disorders or residual risk.
Incorporating these markers into routine clinical practice can enhance the precision of risk assessment and the effectiveness of preventive strategies for Heart Diseases.
